No one goes through medical training so they can disappoint people with lousy outcomes and grievous errors in performing dangerous procedures. Yet, this is happening as a regular course of business in American Medicine. In my post, The Cost of Too Much Spinach, we have a case in point. A young woman suffers from a painful aliment, kidney stones. When she turned to medicine for relief, she was granted a series of tests and surgery that were likely injurious. None of these procedures offered any benefit, not even an accurate diagnosis. Patients like tests, as they believe that a test offers them a definite understanding of their condition. This case shows that tests don’t always perform up to our expectations. Our reliance on technology and invasive procedures illustrate some serious failures in how American medicine is practiced.
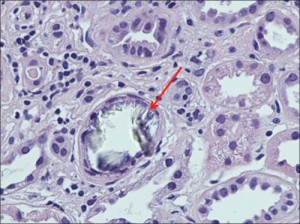
In hindsight, we know that this young woman’s problem was kidney and urethral stones. She had terrible pain in her rib cage on both sides of her body. The local university medical clinic found a 110-degree fever and kidney infection. They performed many tests and also removed her healthy appendix. As Scott Miners wrote in the article I discussed in my previous blog post, the young woman “was very frustrated and still in pain when the clinic staff released her.”
Still in pain, she traveled across the border to Mexico where a naturopathic doctor performed an ultrasound test that found two kidney stones working their way out of her urinary tract. The naturopath’s herbal treatment may have assisted the stones passing and provided relief for the patient.
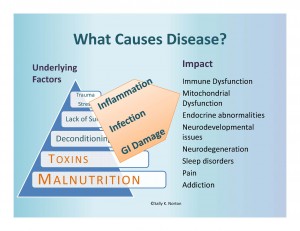
Many questions are raised by this case: Why did the doctors do so many expensive tests and surgery, yet not find the real problem? Are doctors unaware of kidney stones? Do they assume that only old men get kidney stones? Are they aware that kidney stones are becoming increasingly common in females and in children? Are they aware that extreme diets with very high oxalate foods can trigger kidney stones (not to mention other health conditions)? Will they ever consider a person’s diet when they’re trying to determine what’s wrong with their patient?

 no good at all.
no good at all.