PleaseOne of my fellow oxalate-toxicity sufferers alerted me to The Paleo View podcast episode 286 that attempts to “debunk” reports of the health dangers of lectins and oxalates (the oxalate section starts at minute 30). Unfortunately, the episode contains significant errors that serve only to confuse and misinform listeners by perpetuating myths and misunderstandings about oxalate.
The Paleo View’s Spin
The podcast offers this limited perspective: “Listen to us. Don’t bother to learn about oxalate and its connection to health problems. Don’t moderate your intake of oxalate (unless you have major problems with gut health and kidney health).” The cavalier, dismissive attitude leads to a reckless attempt to justify telling you what they think you want to hear: eat all the spinach you want.
Sadly, the opinions and “facts” aired by the Paleo View podcast are based on inadequate contact with (1) medical literature, and (2) real people who are solving and healing mysterious health problems by avoiding spinach and other high oxalate foods.
The cherry-picked views they present ignore the many medically documented harmful effects of oxalate in the body and how these effects play a role in common illnesses. Instead, they prefer to focus inaccurately on the minor issue of oxalates preventing absorption of certain minerals, and on wishful thinking about colon bacteria consuming enough oxalate to save you from oxalate damage. Let me address these two claims.
Minerals Lost to Oxalate
From the very limited perspective of the podcast, the problem with oxalates is that they bind to important nutrient minerals like calcium and prevent them from being absorbed in the gastrointestinal tract from your food. That’s certainly true, and the consequence is that you’re eating less calcium than you think you are when you consume high-oxalate vegetables, for two reasons.
For one, nutritional tables that count up calcium in high-oxalate foods don’t account for the lack of availability of the calcium that is bound up as calcium oxalate. In other words, nutritional analysis of foods does not distinguish calcium oxalate (a toxin) from calcium (the nutrient). They are not interchangeable as far as your body is concerned, yet nutrition claims for calcium in foods treats them as one in the same.
The second problem is that free calcium, magnesium, and iron can all become bound to the oxalic acid (or soluble oxalates) and be lost as nutrients. (The podcast also makes the entirely fanciful claim that gut bacteria break up calcium oxalate, rendering the unavailable calcium available as a nutrient. There is simply no published evidence for that claim.)
Additional Anti-Nutrient Effects Occur After Oxalates are Absorbed
More importantly, the anti-nutrient effects of oxalate go beyond the loss of minerals from foods. There are anti-nutrient effects from the oxalate we do absorb. This happens because the most reactive forms (ions, nanocrystals, and soluble types) get into the body. There they eagerly bind to calcium, iron, and other minerals that are already present in our bodies. This “mineral-stealing” by oxalate is very real concern and does have important “anti-nutrient” consequences. Still, the podcast claims that oxalates “don’t leach minerals from our bodies.”
In the hours after we’ve overloaded on foods with soluble oxalates, oxalate ions will attach to minerals from our foods or from our blood. As a result, these minerals won’t be available for other purposes (like building bone or maintaining proper cellular metabolism). Depending on the amount we eat over time, repeated meal-after-meal intake of oxalate can add up to deficiencies.
Potassium Problems Too
More insidious (and less well known) is the loss of potassium from muscle cells where oxalate crystals are causing inflammation1–3. This sapping of potassium from cells is a third effect, occurring in addition to the oxalate molecules’ first acts of stealing important minerals from both our food and blood4. Our bones, muscles, and other tissues are the ultimate losers as a result of this mineral high-jacking caused by oxalate, which may contribute to systemic problems such as cardiovascular disease, osteoporosis5, and pain syndromes like fibromyalgia.
Which Oxalates Cross the Gut Lining and How Much?
Oxalates absorbed from food clearly present a major challenge to our health. But how much do we absorb from food? The podcast wrongly asserts that we don’t absorb much oxalate from foods like spinach. We absorb plenty.
Estimates of the amount that gets into our bloodstream vary a lot. The classic estimate of typical absorption of oxalate from food is 4—10%. When we absorb more than 10% of what is in our foods, it is called hyper-absorption. Some recent studies suggest that absorbing over 10% may be common. Current estimates suggest that a 50% absorption rate is typical when oxalate intake is very low7. And many studies show that when you eat more, the total amount you absorb goes up. The podcast rightly points out that people with gut absorption problems due to Crohn’s disease, bariatric surgery, IBS, leaky gut, and so on are at higher risk for oxalate hyper-absorption problems8–12.

The question of “soluble” and “insoluble” oxalates is also very important with respect to absorption. The podcast falsely claims that spinach contains mostly insoluble crystals of calcium oxalate that stay inside the digestive tract. In fact, only 28-44% of the oxalates in spinach are insoluble.
Most of the of the oxalates in spinach are soluble (56—72%)15–18 (they are not bound to calcium). Instead the oxalate is oxalic acid or is loosely bound to sodium or potassium. Like the nanocrystals of calcium oxalate, the soluble oxalates easily move though membranes (harming cells in the process). Unlike insoluble calcium oxalate, they easily dissociate into reactive ions. These are the principal forms in which oxalates get into the blood stream, cause metabolic problems, and crystallize in body tissues.
What really matters is this: In absolute terms, the amount of oxalate you ingest is the most important factor influencing how much damage oxalates will cause. Truly, you have no way to know exactly how much oxalate you absorb from your foods. The precautionary approach of limiting how much oxalate you eat is simple and has no intrinsic nutritional risks.
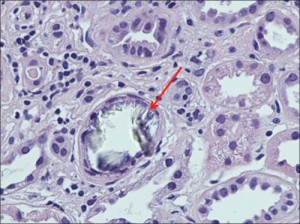
Oxalate Crystals Harm Gut Function
The podcasters do not point out that the insoluble oxalate crystals in plants are a gut irritant13,14. These pointed, sharp microcrystals abrade tissues with a variety of shapes possessing the destructive power of microscopic glassy shards, sand paper, and needles. Chronic abrasions to the gut wall can lead to inflammation and absorption problems. This can set up a vicious cycle making you more susceptible to hyper-absorption and oxalate-realated health problems.
Regardless of the size and shape of crystals, eating less oxalate reduces stress on your gut. Eating less mean fewer nanocrystals and ions are available to damage cells when these ultra-small particles penetrate into and through your gastrointestinal cells. Minimizing inflammation and damage to gut cells (from oxalate AND lectins) may improve your body’s ability to resist the passive movement of the larger oxalate crystals into your blood. Lowering your intake may also help with gut function in general. Many people on the low oxalate diet do better on a gluten free diet as well (less lectins is good for the gut too).
Gut Bacteria Won’t Save You
The Podcast claims that your gut bacteria will protect you from a high oxalate diet. This claim also does not withstand scrutiny. Multiple studies have shown that most people (70% or more) do not have viable gut colonies of oxalobacter formigenes19, a colon-dwelling bacteria which eats oxalate as its primary food.
Oxalate is absorbed throughout the digestive tract, including in the stomach and (primarily) the small intestine20. O. formigenes resides in the colon and only encounters oxalate that has not already been absorbed earlier in the digestive system, or that is released by the body back into the colon. The small proportion of oxalate released back into the colon has already traveled in the blood around the digestive tract and liver. Only a small fraction of this tourist oxalate is sent back into the colon from the blood stream. Given that oxalate ions and nano crystals are so toxic and caustic, this circulation of oxalate can lead to a lot of wear and tear on the digestive tract of people who love spinach, almonds, peanuts, potatoes and other high oxalate foods.
Finally, the podcast also falsely states that eating a high-oxalate diet will encourage the growth of oxalate-eating gut bacteria. There is not much evidence for that claim and no proof that this effect could make oxalate safe to eat. But there is plenty of evidence that if you eat more oxalates (even if you are lucky enough to host a colony of o. formigenes) you will absorb more oxalate (as measured by increased levels in your urine after a meal). People who host o. formigenes will absorb relatively less than people who do not, but they will still absorb more than if they ate lower-oxalate foods. Efforts to re-establish colonies of o. formigenes have to date been unsuccessful.
The lesson is simple: if you want to avoid or recover from possible problems with oxalates, you should eat foods that contain less of them. It’s not hard, it won’t cut you off from essential foods, and it won’t compromise your nutrition. It could change your attitude about which foods you believe are health-giving, however. This may be the tragedy the Paleo View wants to protect you from.
Choosing Low Oxalate Foods Is Healthy and Nourishing
The podcast vigorously promotes the myth that low-oxalate eating means you have to give up “good” vegetables and therefore you can’t get proper nutrition. Nothing could be more wrong. That view (also promulgated by some kidney specialists who haven’t bothered to find out what foods have oxalates) goes back to the days when people presumed that all greens were high in oxalate. There are plenty of greens and other vegetables that are low oxalate when eaten in reasonable portions (1 C raw or ½ C cooked are typical serving sizes.)
There is no dietary reason that low-oxalate eaters risk being more malnourished than those eating a high-oxalate diet. I suspect that the opposite is a more likely scenario. Of course, no one has offered sound evidence that any vegetables or nuts or potatoes are essential to being well-nourished and healthy. The urgency to defend a plant-based diet, especially one based on high-oxalate foods, originates primarily from science that is increasingly being revealed as flawed (e.g. that animal fats are intrinsically bad for you) and from cultural prejudices that have essentially no basis in science (e.g. that farming animals is more unsustainable or environmentally destructive than farming plants).
But you don’t have to give up plants (or even a mostly plant-based diet) to successfully control your oxalate consumption. Anyone who says otherwise is just trying to scare you into staying ignorant of the danger.
Wishes vs. Facts
Being accurately informed is a necessary step before you can take deliberate, sensible actions to lower the risks that may be present in your own situation and dietary practices. Accurate information is not something the Paleo View wants you to have. They’d rather you trust their preferences, biases, and instincts.
Clearly, they do not want your faith in spinach to be shaken. Heaven forbid! And they don’t want you to consider that a life without spinach may lead to less pain, stronger bones, and many other happy outcomes—as it has for (at least) tens of thousands of actual people.
My Conclusion about Their Conclusions
The Paleo View podcast encourages listeners to ignore the evidence of serious health problems caused by excessive oxalate consumption. Their logic is this: since there is no proof that everyone is harmed by oxalate in foods like spinach, you should eat as much as you like and ignore the possibility that it could be harmful. How tragic indeed if the misinformation in this podcast discourages people from considering, let alone trying, an oxalate-aware eating strategy.
No need to fall victim to myths and misunderstandings about oxalate.
More details here, here, here, and here.
Key Points
Minerals are lost from foods and the body due to high oxalate content of our diets.
Oxalate causes gut damage, and damage to other organs too.
Spinach has a lot of soluble oxalate in it.
Bacteria that degrade oxalate are in short supply, cannot be replaced with probiotics and can only do so much to protect us from high oxalate foods.
A low oxalate diet can be perfectly nourishing and safe. We have no nutritional requirement to eat any high oxalate food.
Defending the frequent consumption of spinach is a disservice to listeners.
References
- Mulay SR, Anders H-J. Crystallopathies. N Engl J Med. 2016;374(25):2465-2476.
- Mulay SR, Kulkarni OP, Rupanagudi KV, Migliorini A, Darisipudi MN, Vilaysane A, Muruve D, Shi Y, Munro F, Liapis H, Anders H-J. Calcium oxalate crystals induce renal inflammation by NLRP3-mediated IL-1β secretion. J Clin Invest. 2013;123(1):236-246. doi:10.1172/JCI63679.
- Franklin BS, Mangan MS, Latz E. Crystal Formation in Inflammation. Annu Rev Immunol. 2016;34(1):173-202. doi:10.1146/annurev-immunol-041015-055539.
- Muñoz-Planillo R, Kuffa P, Martínez-Colón G, Smith BL, Rajendiran TM, Núñez G. K+ efflux is the common trigger of NLRP3 inflammasome activation by bacterial toxins and particulate matter. Immunity. 2013;38(6):1142-1153. doi:10.1016/j.immuni.2013.05.016.
- Shavit L, Girfoglio D, Vijay V, Goldsmith D, Ferraro PM, Moochhala SH, Unwin R. Vascular calcification and bone mineral density in recurrent kidney stone formers. Clin J Am Soc Nephrol CJASN. 2015;10(2):278-285. doi:10.2215/CJN.06030614.
- Holmes RP, Goodman HO, Assimos DG. Contribution of dietary oxalate to urinary oxalate excretion. Kidney Int. 2001;59(1):270-276. doi:10.1046/j.1523-1755.2001.00488.x.
- Holmes RP, Knight J, Assimos DG. Lowering urinary oxalate excretion to decrease calcium oxalate stone disease. Urolithiasis. 2016;44(1):27-32. doi:10.1007/s00240-015-0839-4.
- Canos HJ, Hogg GA, Jeffery JR. Oxalate nephropathy due to gastrointestinal disorders. Can Med Assoc J. 1981;124(6):729-733.
- Cartery C, Faguer S, Karras A, Cointault O, Buscail L, Modesto A, Ribes D, Rostaing L, Chauveau D, Giraud P. Oxalate Nephropathy Associated with Chronic Pancreatitis. Clin J Am Soc Nephrol CJASN. 2011;6(8):1895-1902. doi:10.2215/CJN.00010111.
- Froeder L, Arasaki CH, Malheiros CA, Baxmann AC, Heilberg IP. Response to Dietary Oxalate after Bariatric Surgery. Clin J Am Soc Nephrol CJASN. 2012;7(12):2033-2040. doi:10.2215/CJN.02560312.
- Hueppelshaeuser R, von Unruh GE, Habbig S, Beck BB, Buderus S, Hesse A, Hoppe B. Enteric hyperoxaluria, recurrent urolithiasis, and systemic oxalosis in patients with Crohn’s disease. Pediatr Nephrol Berl Ger. 2012;27(7):1103-1109. doi:10.1007/s00467-012-2126-8.
- Kumar R, Lieske JC, Collazo-Clavell ML, Sarr MG, Olson ER, Vrtiska TJ, Bergstralh EJ, Li X. Fat Malabsorption and Increased Intestinal Oxalate Absorption are Common after Rouxen-Y Gastric Bypass Surgery. Surgery. 2011;149(5):654-661. doi:10.1016/j.surg.2010.11.015.
- Altin G, Sanli A, Erdogan BA, Paksoy M, Aydin S, Altintoprak N. Severe destruction of the upper respiratory structures after brief exposure to a dieffenbachia plant. J Craniofac Surg. 2013;24(3):e245-247. doi:10.1097/SCS.0b013e318286068b.
- Konno K, Inoue TA, Nakamura M. Synergistic defensive function of raphides and protease through the needle effect. PloS One. 2014;9(3):e91341. doi:10.1371/journal.pone.0091341.
- Bong W-C, Vanhanen LP, Savage GP. Addition of calcium compounds to reduce soluble oxalate in a high oxalate food system. Food Chem. 2017;221:54-57. doi:10.1016/j.foodchem.2016.10.031.
- Brogren M, Savage GP. Bioavailability of soluble oxalate from spinach eaten with and without milk products. Asia Pac J Clin Nutr. 2003;12(2):219-224.
- The Low Oxalate Diet Addendum Winter 2010 – Numerical Values Table. VP Found Newsl. 2010;(33):18-23.
- The Low Oxalate Diet Addendum Summer 2012 – Numerical Values Table. VP Found Newsl. 2012;(37):6-9, 19-25.
- Barnett C, Nazzal L, Goldfarb DS, Blaser MJ. The Presence of Oxalobacter formigenes in the Microbiome of Healthy Young Adults. J Urol. 2016;195(2):499-506. doi:10.1016/j.juro.2015.08.070.
- Hautmann RE. The stomach: a new and powerful oxalate absorption site in man. J Urol. 1993;149(6):1401-1404.