Today’s health crisis. Have you noticed it? Obesity, insulin resistance, diabetes, kidney disease, cancer, infertility, behavioral and mood problems, poor sleep, and PAIN. Do you know anyone with any of these problems? Yes, you do, even if you are not aware of it. And, the suffering is happening at younger and younger ages. Our kids are in trouble, we’re all in trouble.
It is expensive to be sick. Both time and money are sucked out of our lives, not to mention the fun. And what about the bigger picture all around us? Perhaps you’ve noticed that poor health is threatening social and economic stability, world-wide.
Eating Better?
So, what are we doing about it? Eating better? Going “natural”? Yes, we are indeed eating more veggies and less meat, less fat too. We’re swearing off gluten and 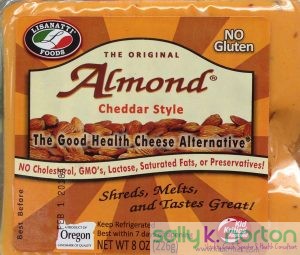 milk, going for alternative low-carb or gluten-free breads, alternative “milk”, and fake cheese. Is this going to save us? I say no. Hear about one reason why this approach is not a great solution: in this video about oxalate toxicity from natural foods.
milk, going for alternative low-carb or gluten-free breads, alternative “milk”, and fake cheese. Is this going to save us? I say no. Hear about one reason why this approach is not a great solution: in this video about oxalate toxicity from natural foods.
My Ancestral Health Symposium Presentation
In September, I had an opportunity to offer an address to the Ancestral Health Society. This presentation argues that many of today’s health foods are having the opposite of the intended effect. Rather than making us healthier, the superfood food craze could, like the holy war against saturated fat, be launching another public health calamity, as expensive and unpleasant as the current diabetes and obesity explosion.
Here are some highlights from this talk:
- Low-level toxicity and nutrient deficiencies make us sick.
- One of the most potent toxins that people regularly ingest in the contemporary diet is oxalate.
- Oxalate causes nutrient depletion AND toxicity in the body.
- Oxalate, when purified, can rapidly kill a person.
- It was even the poison of interest in the very first experimental toxicology study published in 1823 in England, because it caused several accidental deaths in the early1800s.
- Many of the plant foods we like to think are good for us have enough oxalate to harm our health in much more subtle ways.
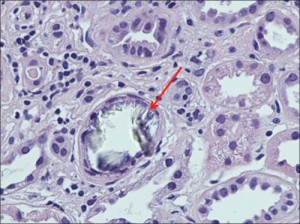
- These natural foods might even cause mechanical abrasion to your digestive tract do to the “needle effect”.
- Oxalate can collect in your tissues.
- The availability of high oxalate foods we see today is unprecedented.
- Today we are eating oxalate in amounts that cause us to begin accumulating oxalate in our arteries, bones, thyroid, breasts, and kidneys.
- When you eat “normal” levels of oxalate, you “maintain” and grow the oxalate deposits that have already started in your body.
- Medical and nutrition authorities have virtually no awareness of the threat of biological toxicity posed by over-exposure to oxalate and its precursors. They are not paying attention to the increase in our use of high oxalate foods.
- Going low destabilizes oxalate in the body, and helps it move out.
- Going low can prevent and even reverse a lot of common complaints, as proven by thousands of reports from real people in the real world (members of the VP Foundation, Participants in the Trying Low Oxalates online groups, my own clients and followers, and many others).
Action Items for You
- Please watch the video, it is only 39 minutes and is packed with helpful images and information that will make you want to share it and watch it a second time.
- Please give it a thumbs up.
- Share with those you love.
- Let me know what you think.
… and
- Skip the swiss chard and almonds.
The fewer toxins in your body the better, even the natural ones!
“From a practical point of view, it would be better to avoid oxalate-rich foods than to take measures to neutralize the effect of oxalic acid, especially when other sources of green vegetables are available.”
—Hoover and Karunairatnam (1945).
Oxalate content of some leafy green vegetables and its relation to oxaluria and calcium utilization.
The Biochemical Journal 39, 237.