If you are taking 500 mg or more vitamin C daily, there is something you need to know. Vitamin C (in excess) can become a toxin that can lead to kidney stones, arthritis, other pain conditions, and perhaps, compromised brain function. For decades we have been told that vitamin C is good for us and may help prevent colds. But too much of a good thing can make trouble. (Research has not been able to confirm the theory that vitamin C supplements help to prevent colds unless you routinely engage in physically demanding work or endurance sports.) [Read more…]
Standing on Steady Ground: Resisting New Ideas
 Most people will find certainty and safety by subscribing to widely held ideas, regardless of the “truth” of those ideas. Likewise, institutions and the people that are governed by them resist new explanations for phenomena. A classic example of this is found in the dawn of two radical ideas that 1) the earth moves around in space, and 2) the earth revolves around the sun. [Read more…]
Most people will find certainty and safety by subscribing to widely held ideas, regardless of the “truth” of those ideas. Likewise, institutions and the people that are governed by them resist new explanations for phenomena. A classic example of this is found in the dawn of two radical ideas that 1) the earth moves around in space, and 2) the earth revolves around the sun. [Read more…]
Letting Patients Down
No one goes through medical training so they can disappoint people with lousy outcomes and grievous errors in performing dangerous procedures. Yet, this is happening as a regular course of business in American Medicine. In my post, The Cost of Too Much Spinach, we have a case in point. A young woman suffers from a painful aliment, kidney stones. When she turned to medicine for relief, she was granted a series of tests and surgery that were likely injurious. None of these procedures offered any benefit, not even an accurate diagnosis. Patients like tests, as they believe that a test offers them a definite understanding of their condition. This case shows that tests don’t always perform up to our expectations. Our reliance on technology and invasive procedures illustrate some serious failures in how American medicine is practiced.
In hindsight, we know that this young woman’s problem was kidney and urethral stones. She had terrible pain in her rib cage on both sides of her body. The local university medical clinic found a 110-degree fever and kidney infection. They performed many tests and also removed her healthy appendix. As Scott Miners wrote in the article I discussed in my previous blog post, the young woman “was very frustrated and still in pain when the clinic staff released her.”
Still in pain, she traveled across the border to Mexico where a naturopathic doctor performed an ultrasound test that found two kidney stones working their way out of her urinary tract. The naturopath’s herbal treatment may have assisted the stones passing and provided relief for the patient.
Many questions are raised by this case: Why did the doctors do so many expensive tests and surgery, yet not find the real problem? Are doctors unaware of kidney stones? Do they assume that only old men get kidney stones? Are they aware that kidney stones are becoming increasingly common in females and in children? Are they aware that extreme diets with very high oxalate foods can trigger kidney stones (not to mention other health conditions)? Will they ever consider a person’s diet when they’re trying to determine what’s wrong with their patient?
The Cost of Too Much Spinach
In the July-August issue of Well Being Journal, Scott Miners1 shared the story of a teenager who went through a series of expensive diagnostic tests and unnecessary surgery. She had extreme pain and difficulty urinating. Four MRIs, 2 CT scans, and x-rays failed to detect her kidney-urethra stones. Without a correct diagnosis, they removed her healthy appendix. None of these medical procedures offered any relief.
This young woman suffered a great deal of pain, underwent dangerous surgery, and must have missed out on normal life activities due to kidney stones. Kidney stones are becoming more common, especially in women and the young. Yet, in this case, the best tests of modern medicine failed to detect them. Still, there were bills to be paid.
The costs of these tests vary a lot, in the table below I roughly estimate the expenses generated by this medical “wild goose chase”. Her kidney stone trouble may have generated nearly $50,000 in medical expenses, and they did her  no good at all.
no good at all.
Sadly, she was never told, until after Scott read my article, that eating too much oxalate from spinach could be a risk factor for kidney stones. Scott writes: “… she said she had become a vegetarian four years earlier and had been eating massive amounts of spinach in those years, prior to the kidney stone formation.” Her likely purpose in eating spinach was to support her health, and not to make her sick and broke!
| Medical Procedure | Number Performed | Cost Range | Total Estimated Mean Cost |
|---|---|---|---|
| MRI $1,500 – $5,000 | 4 | 6,000 – 20,000 | 13,000 |
| CT Scan $500 – $1,200 | 2 | 1,000 – 2,400 | 1,700 |
| X-ray $300 – $600 | 1 | 300 – 600 | 450 |
| Appendectomy Surgery median cost is $33,0002 | 1 | 33,000 | |
| TOTAL: | $48,150 |
References:
- Miners, S. Kidney Stones and High-Oxalate Foods. Well Being Journal. 24:4, (2015).
- Hsia RY, Kothari AH, Srebotnjak T & Maselli J. Health care as a ‘market good’? appendicitis as a case study. Intern. Med. 172, 818–819 (2012).
Catastrophic Complication of Weight-Loss Surgery: Kidney Failure

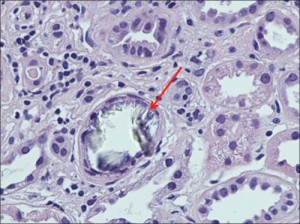
Figure 1 Nagaraju (2013). Large intraluminal translucent crystals of calcium oxalate, tubular epithelial degeneration (foamy cytoplasm, pyknosis, karyorrhexis, indistinct cell borders, dilated lumina), lymphocytic infiltration in the interstitium (H and E, ×400)
A case of kidney failure after bariatric surgery is stopped with low-oxalate diet.
Canadian nephrologists reported a case of life-threatening kidney damage caused by kidney deposits of oxalate crystals.1 The doctors performed a kidney biopsy on their patient, a 54-year old man, 20 months after duodenal switch weight-loss surgery. His blood creatinine levels had tripled over the previous nine months. The biopsy found oxalate crystals causing tubular damage and atrophy, fibrosis, and inflammation. They also noted hardening of the blood-filtering glomerular capillaries.
The patient was treated with a low-oxalate diet, calcium citrate (1,000 mg 3 times a day with meals), high water consumption, and the drug cholestyramine to help reduce oxalate absorption. This stabilized his blood creatinine levels and his urine oxalate dropped by a third from 99 to 63mg per day. Normal urine oxalate is under 40-45 mg/day. The authors’ want practicing clinicians to be aware of the increased risk of excessive absorption of oxalates from food following weight-loss surgery (“secondary enteric hyperoxaluria”) which can lead to kidney stones and life-threatening renal failure due to oxalate-induced kidney damage.
This case illustrates: 1) changes to gut function can alter oxalate absorption; 2) oxalates in foods can cause tissue damage; and 3) this process may be arrested by limiting oxalate absorption with a low-oxalate diet and supportive therapies.
Interestingly, this patient’s urine oxalate levels, although lower, remained elevated (63mg/day) despite effective diet therapy. Consistent with reports from cases of genetic oxalosis, this may indicate that the patient’s tissues are shedding existing oxalate deposits in the kidney and elsewhere in the body. The clearing of oxalate deposits may contribute to urinary oxalate, perhaps for years. It is likely that shrinking tissue oxalate deposits leave in their wake persistent renal scarring and tissue damage elsewhere.
Oxalate deposits can develop over time after either Roux-en-Y gastric bypass surgery (RYGB) or duodenal switch surgery. These surgeries can trigger an increase in the absorption of dietary oxalates (perhaps due to bile salts in the colon and fat malabsorption in the small intestine). This potential complication -the possibility of increased oxalate absorption leading to high urine oxalates and, eventually, kidney failure – is not typically discussed at the time of consent to surgery.2 Nor are these patients typically told that they can minimize the risk by modifying their diet to avoid oxalates in foods. Discharge and follow-up counseling and education should include instructions for the low-oxalate diet. The gastric banding procedure is not likely to cause this problem.2
Oxalate deposits in the body develop gradually and often without symptoms.3 Although rarely prescribed by clinicians, a low oxalate diet can help avert the risk of too much oxalate and may be especially important for people with intestinal and digestive problems, including, but not limited to weight-loss surgery.4 Other surgical procedures (intestinal resection, ileostomy, bladder diversion surgery) and GI conditions such as irritable bowel syndrome (IBS), celiac disease, Crohn’s disease, small intestinal bacterial overgrowth (SIBO), pancreatic insufficiency, or poor fat digestion (steatorrhea) can also contribute to excessive absorption of oxalates in the digestive tract.
The renal damage caused by oxalates may not be reversible so it is important to start the low oxalate diet as early as possible. Anyone who is increasing their water intake or taking calcium citrate to reduce absorption of oxalates needs to be aware that timing is important. Water with meals can increase oxalate absorption, so drink fluids between meals. Also, calcium citrate tablets need time to dissolve, so take them about 20 minutes before meals to maximize the oxalate sequestration effects.
Key Point: Dietary oxalates can cause kidney failure after bariatric surgery. The progression of the disease can be halted by the low-oxalate diet, if implemented correctly and early enough.
For my low-oxalate grocery shopping list click here.
References
- Nagaraju SP, Gupta A, McCormick B. Oxalate nephropathy: An important cause of renal failure after bariatric surgery. Indian J Nephrol. 2013;23(4):316-318. doi:10.4103/0971-4065.114493.
- SenthilKumaran S, David SS, Menezes RG, Thirumalaikolundusubramanian P. Concern, counseling and consent for bariatric surgery. Indian J Nephrol. 2014;24(4):263-264. doi:10.4103/0971-4065.133045.
- Marengo S, Zeise B, Wilson C, MacLennan G, Romani AP. The trigger-maintenance model of persistent mild to moderate hyperoxaluria induces oxalate accumulation in non-renal tissues. Urolithiasis. 2013;41(6):455-466. doi:10.1007/s00240-013-0584-5.
- Lieske JC, Tremaine WJ, De Simone C, et al. Diet, but not oral probiotics, effectively reduces urinary oxalate excretion and calcium-oxalate supersaturation. Kidney Int. 2010;78(11):1178-1185. doi:10.1038/ki.2010.310.
Further Reading about Bariatric Surgery and Oxalates
- Agrawal V, Liu XJ, Campfield T, Romanelli J, Enrique Silva J, Braden GL. Calcium oxalate supersaturation increases early after Roux-en-Y gastric bypass. Surg Obes Relat Dis Off J Am Soc Bariatr Surg. 2014;10(1):88-94. doi:10.1016/j.soard.2013.03.014.
- Ahmed MH, Byrne CD. Bariatric surgery and renal function: a precarious balance between benefit and harm. Nephrol Dial Transplant. 2010;25(10):3142-3147. doi:10.1093/ndt/gfq347.
- Asplin JR. Hyperoxaluria and Bariatric Surgery. In: AIP Conference Proceedings. Vol 900. AIP Publishing; 2007:82-87. doi:10.1063/1.2723563.
- Froeder L, Arasaki CH, Malheiros CA, Baxmann AC, Heilberg IP. Response to Dietary Oxalate after Bariatric Surgery. Clin J Am Soc Nephrol CJASN. 2012;7(12):2033-2040. doi:10.2215/CJN.02560312.
- Kumar R, Lieske JC, Collazo-Clavell ML, et al. Fat Malabsorption and Increased Intestinal Oxalate Absorption are Common after Rouxen-Y Gastric Bypass Surgery. Surgery. 2011;149(5):654-661. doi:10.1016/j.surg.2010.11.015.
- Lieske JC, Mehta RA, Milliner DS, Rule AD, Bergstralh EJ, Sarr MG. Kidney stones are common after bariatric surgery. Kidney Int. October 2014. doi:10.1038/ki.2014.352.
- Nasr SH, D’Agati VD, Said SM, et al. Oxalate Nephropathy Complicating Roux-en-Y Gastric Bypass: An Underrecognized Cause of Irreversible Renal Failure. Clin J Am Soc Nephrol CJASN. 2008;3(6):1676-1683. doi:10.2215/CJN.02940608.
- Patel BN, Passman CM, Fernandez A, et al. Prevalence of Hyperoxaluria After Bariatric Surgery. J Urol. 2009;181(1):161-166. doi:10.1016/j.juro.2008.09.028.
- Ritz E. Bariatric surgery and the kidney – Much benefit, but also potential harm. Clin Kidney J Clin Kidney J. 2013;6(4):368-372.
- Whitson JM, Stackhouse GB, Stoller ML. Hyperoxaluria after modern bariatric surgery: case series and literature review. Int Urol Nephrol. 2010;42(2):369-374. doi:10.1007/s11255-009-9602-5.
I missed a key footnote in college about oxalates in food
Sweet potatoes, walnuts, and kiwi are no longer my friends. Apparently, they never were. I just never got the memo.
My nutrition education hadn’t warned me that a variety of vegetables, nuts, and fruits could cause health problems due to their oxalate content. Instead, my college textbooks suggested that toxic oxalate is confined to a short list of five foods. My old Basic Food text states: “… oxalic acid, which occurs in spinach, chard, beet greens, and rhubarb, is toxic” (p.17)1. Another textbook, Normal and Therapeutic Nutrition, added coco to this same list, bringing the total up to five foods with oxalic acid (p. 134)2. Later in the therapeutic section of Normal and Therapeutic Nutrition, the authors added 15 more foods to the list in the one and only paragraph devoted to dietary restriction of oxalate (p. 675). The oxalate-restricted diet is described in under 60 words.
Truth be told, lab methods for measuring oxalate in foods did not become reliable until about 1980. Today in 2015, the nutrition profession still lacks complete or accurate reference for the oxalate content of foods and supplements. And, we have not fully described or tested the hypothetical oxalate-restricted diet, because we lack sufficient data and other tools needed to do so. Such a diet can only be created by an opt-in method of building a diet with foods that have been accurately tested for oxalate content. Given the ubiquitous nature of oxalate in foods, the old notion of avoiding the top 20 high-oxalate foods is illogical and mathematically unsound. Yet, this is exactly the standard of practice today. In the rare instance when the oxalate-restricted diet is prescribed, the patient is handed an inaccurate list of the highest oxalate containing foods and told to limit these foods to occasional, moderate portions.
The chief message contained in my college text books about oxalic acid in foods is this: Oxalic acid reduces the amount of calcium that can be absorbed from very high oxalate foods to nearly zero, although the food composition reference tables list spinach and other greens as containing calcium, in significant amounts. From a nutritional standpoint these foods lack calcium because it is bound to oxalic acid and cannot be used by the body. These two textbooks disagree about the resulting loss of calcium availability as a result of adding chocolate (oxalic acid) to milk. When I was in school designing menus to meet nutritional requirements laid out by the FDA, we were not graded down for including, and counting, un-available calcium (in known high oxalate foods) in our meal plans. Oxalate was considered a non-issue back then, and still is today. In fact, high-oxalate foods are widely and loudly promoted as healthy foods.
My college textbooks also reassured me that oxalic acid “does not cause illness in the amounts that are normally consumed”. In today’s world proclaiming the healthy virtues of veganism, raw foods, and vegetable juicing, this dismissive and untested assertion sounds irresponsible. There is a growing body of evidence that oxalates can accumulate in tissues, not just the kidneys, which can lead to a variety of connective tissue and other problems in susceptible individuals. My Basic Foods book promoted the idea of increasing consumption of fruits and vegetables without a thought to the possibility that people could get into trouble with excessive amounts of naturally occurring oxalate in their foods. It didn’t occur to them that I had (while in college) a garden patch of Swiss chard which I ate in large portions every day for 2 months. At the time I was using crutches and 3600mg of ibuprofen to curb the constant foot pain that persisted after having surgery on both of my feet three years earlier in 1986. Today, I am pretty sure about the reason my feet were not healing properly – the toxic oxalic acid in my vegetarian diet and already in my body was interfering with healing.
So the seed was never planted in my head while in college, that over-doing Swiss chard and other high-oxalate foods could be trouble. It turns out that it can bring one’s productive life to a halt, as it did mine – several times.
References
- June C. Gates. Basic Foods. (Holt, Rinehart and Winston, 1981).
- Corinne H. Robinson & Marilyn R. Lawler. Normal and Therapeutic Nutrition. (Macmillan Publishing Co. Inc., 1982).
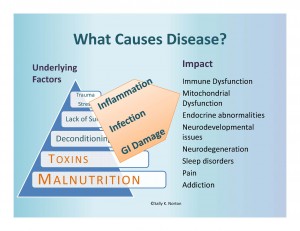
What is making us sick?
Nutritional deficiencies and excessive exposure to toxins, both natural and man made are at the root of our health problems. These issues must be addressed to reverse disease.
Sugar
Sugar, Sugar Everywhere
Tis the season for hooking you on sugar.
Getter hyper-jazzed on sugar is optional.
Christmas is a holiday about new beginnings and the magic and wonder of ordinary life. Intentionally placed at the winter solstice, Christmas, like the solstice marks the end of the ever shortening days. Finally, the days are getting longer again. Still it is the dark time, and a time to cheer each other. So, off we go retail treasure-hunting and stuffing ourselves with sugar. We are easy prey for merchants of all stripes who coat the checkout with sugar in its many forms seductively dressed in both nostalgia and novelty. Peppermint bark, and other “sugarplums” so everywhere, so obtainable, promise to fulfill longings you didn’t know you had.
Do you resist? Are you successfully avoiding candy, cookies, and the like? If so, does it leave you feeling left out?
Want a simple treat without damaging your health in the process?
Try ultra humble and easy baked apples (see post with recipe)
Tip: good food tastes best when you are hungry. Brain-numbing sugars, on the other hand, excite the senses even when you are full and over-fed. This turns “food” into an addictive substance from which you have no natural defenses. You need a plan for maintaining your sanity, waist-line, and good sense.